Understanding The Four Phases of Your Menstrual Cycle
Have you ever noticed that some weeks you feel clear-headed, confident, and energized—while other weeks feel heavier, more emotional, or simply days being harder to get through? If you’ve ever wondered why your energy, emotions, focus, or patience seem to fluctuate from week to week, you’re not imagining it—and you’re not “too sensitive.”
For many people with menstrual cycles, these shifts are deeply connected to hormonal changes that happen every month.Understanding your menstrual cycle can be a powerful act of self-compassion.Instead of judging yourself for feeling “off,” you can begin to recognize patterns, honor your needs, and respond with care.
Your menstrual cycle is a complex, hormone-guided process that influences not only your reproductive system, but also your nervous system, mood regulation, sleep, appetite, and stress response. From a therapeutic perspective, understanding your cycle can be an empowering way to replace self-criticism with self-attunement.
Rather than asking, “What’s wrong with me?”
We can begin asking, “What phase am I in—and what might my body be asking for?”
Let’s gently walk through the four phases of the menstrual cycle—biologically, emotionally, and therapeutically.
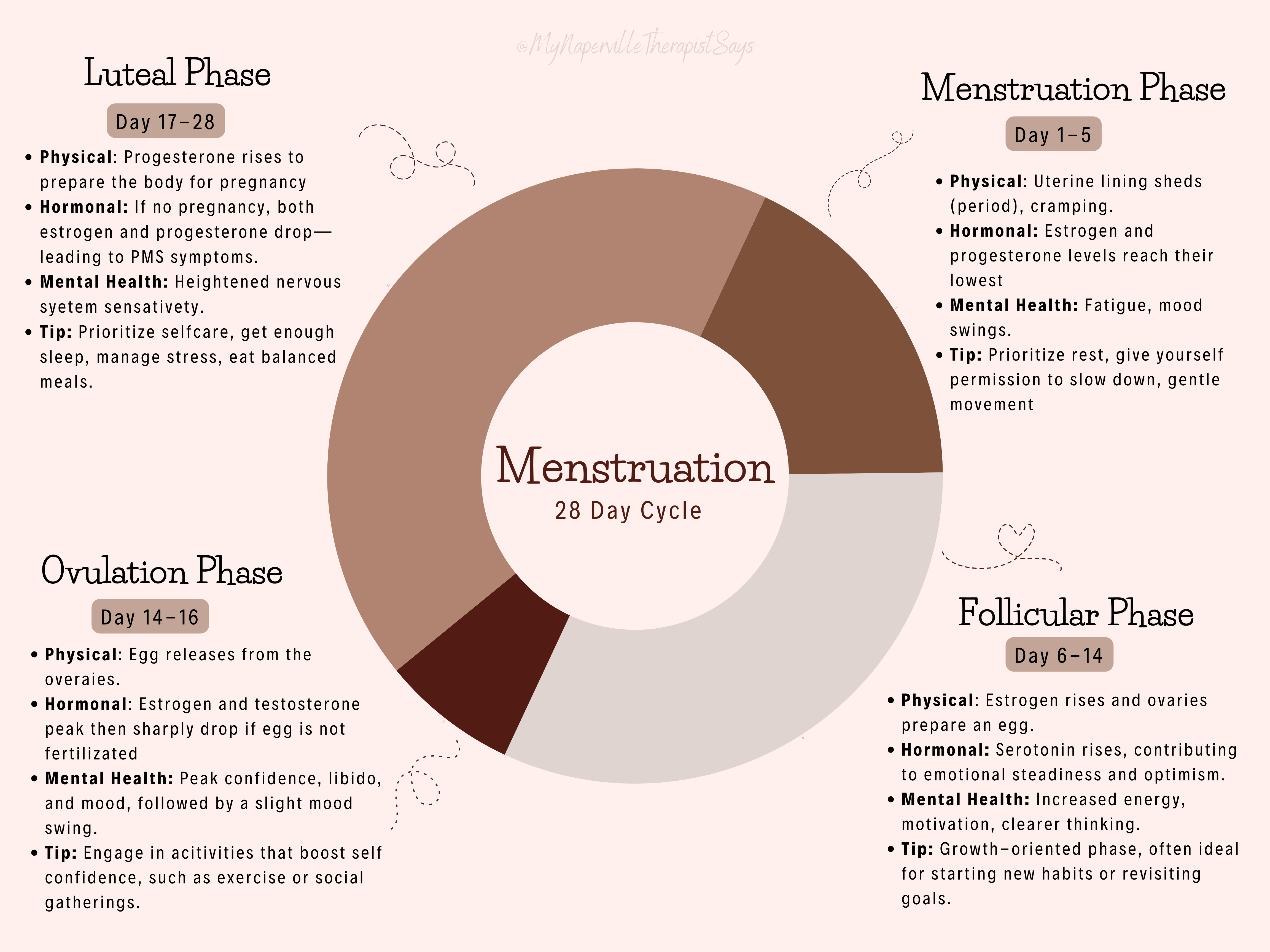
Phase One: The Menstrual Phase (Days 1–5)
Theme: Rest, Release, and Reflection
What’s happening biologically
The menstrual phase begins on the first day of bleeding. The body sheds the uterine lining as estrogen and progesterone levels reach their lowest point in the cycle. There is also a temporary dip in serotonin, a neurotransmitter involved in mood regulation. During this phase, the body actively sheds the old endometrial lining through an inflammatory process driven by rapid hormonal shifts. As the uterus releases this tissue, it begins repairing itself and preparing to rebuild the lining while new ovarian follicles start to develop.Low estrogen and progesterone levels mean the body must expend extra energy managing the inflammation, often resulting in fatigue and a greater need for rest.
This combination can impact energy, pain perception, and emotional resilience.
Common physical and emotional experiences
- Fatigue or low motivation
- Cramps, headaches, or body aches
- Increased emotional sensitivity
- Sadness, irritability, or tearfulness
- A desire to withdraw or be quieter
Clinically, this phase can coincide with reduced cognitive stamina and increased nervous system sensitivity.
Therapeutic reframe
This is not a “low-functioning” phase—it is a low-output phase. Your body is doing meaningful internal work.
Gentle ways to support yourself:
- Prioritize rest and give yourself permission to slow down
- Stay hydrated and nourish your body with iron-rich foods
- Use heat (like a heating pad) to ease discomfort
- Engage in gentle movement, such as stretching, yoga, or short walks
Therapy-friendly support:
This can be a powerful phase for reflection rather than productivity. It’s a good time to:
- Check in with your emotional world
- Reflect on boundaries and needs
- Focus on essential tasks only
- Practice self-soothing and grounding techniques
Think of this phase as a reset, not a setback.
This phase invites permission to do less and feel more.
Phase Two: The Follicular Phase (Days 6–14)
Theme: Renewal, Motivation, and Possibility
What’s happening biologically
As menstruation ends, estrogen begins to rise. The brain releases follicle-stimulating hormone (FSH), prompting the ovaries to prepare an egg.Increased estrogen supports improved mood, focus, and energy.
Serotonin levels also tend to rise, contributing to emotional steadiness and optimism.
Common physical and emotional experiences
- Increased energy and motivation
- Clearer thinking and improved concentration
- Sociability and openness
- Hopefulness or excitement
This is often a phase of forward momentum.
Therapeutic reframe
This is a growth-oriented phase, often ideal for starting new habits or revisiting goals.
Serotonin (a “feel-good”neurotransmitter) often increases during this phase, which can support emotional resilience and confidence.
Gentle ways to support yourself:
- Take advantage of motivation to begin projects or make plans
- Engage in social activities and movement
- Practice goal-setting or mindfulness
- Eat balanced meals to support steady energy
Therapy-friendly support:
This is often a great phase for:
- Exploring goals and aspirations
- Building routines or habits
- Engaging in deeper therapeutic work
- Leaning into curiosity and growth
This phase often carries a sense of possibility—a natural time to plant seeds.
Phase Three: Ovulation (Days 14–16)
Theme: Connection, Expression, and Confidence
What’s happening biologically
Ovulation occurs when a surge in luteinizing hormone (LH) releases an egg from the ovary. Estrogen and testosterone peak, influencing mood, libido, and confidence.
Shortly after ovulation, if no pregnancy occurs these hormones drop sharply, and the egg along with its supporting hormones, start to break down and are reabsorbed by the body. Which is a noticeable feeling form most.
Common physical and emotional experiences
- Increased confidence and self-expression
- Heightened libido or relational desire
- Sociability and verbal ease
- Occasionally increased anxiety or overstimulation
Therapeutic reframe
This phase often highlights interpersonal energy—how you connect, communicate, and assert yourself.
Gentle ways to support yourself:
- Schedule important conversations or social plans
- Maintain steady nutrition and hydration
- Practice stress-relief techniques like deep breathing or meditation
- Balance stimulation with moments of grounding
Therapy-friendly support:
This phase can be supportive for:
- Strength-based reflection
- Celebrating progress and resilience
- Navigating relationships and communication
- Gently noticing any anxiety without judgment
This phase often invites connection—with yourself and others and to be seen and heard.
Phase Four: The Luteal Phase (Days 17–28)
Theme: Sensitivity, Integration, and Self-Compassion
What’s happening biologically
After ovulation, progesterone rises to prepare the body for pregnancy.Progesterone can affect the nervous system, digestion, sleep, and emotional regulation.
If pregnancy does not occur, the body withdraws hormonal support with a drop in both estrogen and progesterone—often leading to mood instability and PMS symptoms.
Common physical and emotional experiences
- Fatigue or brain fog
- Mood swings or emotional vulnerability
- Anxiety, sadness, or irritability
- Changes in appetite or sleep
- Heightened sensitivity to stress
For some, these changes are mild. For others, they may be intense or distressing (including PMDD).
Therapeutic reframe
This phase is not a failure of coping—it is a period of heightened nervous system sensitivity. This being defines as a time when the nervous system is more reactive because hormone levels are changing quickly, calming neurotransmitter support becomes less predictable, and stress pathways are more easily activated.
Stress response is more easily triggered: Lower estrogen reduces serotonin and dopamine support, while cortisol responses may feel stronger—making the nervous system more reactive to stress, noise, emotions, and sensory input. Not only are emotions heightened, but along with physical sensitivity and sleep disturbances
Gentle ways to support yourself:
Reduce caffeine and excess sugar
- Prioritize sleep and rest
- Engage in light movement like stretching or walking
- Practice calming techniques (breathing, meditation, grounding)
- Nourish your body with magnesium- and B6-rich foods
Therapy-friendly support:
This phase benefits from:
- Increased patience and self-compassion
- Emotional validation and check-ins
- Reducing expectations and external pressure
- Focusing on comfort, safety, and regulation
For some, symptoms during this phase may be more intense (such as with PMS or PMDD). If mood changes significantly interfere with daily life or relationships, support from a healthcare provider or therapist can be incredibly helpful.
This phase asks for kindness, not correction.
A Gentle Reminder
Your menstrual cycle is not something to “fix.” It’s a rhythm your body moves through—one that changes across the lifespan and varies from person to person. Your experience is valid, even if it looks different from someone else’s.
Learning your cycle can help you:
- Release self-blame
- Better understand emotional patterns
- Advocate for your needs
- Build a more compassionate relationship with your body
You don’t need to be productive, cheerful, or consistent every day of the month. You’re allowed to ebb and flow.
A Note for Partners:
How to Offer Support Across the Menstrual Cycle
If you love or care for someone who menstruates, understanding the menstrual cycle can be a meaningful way to strengthen your relationship. Hormonal shifts can influence energy levels, emotional sensitivity, stress tolerance, and communication style—but these changes are not character flaws, overreactions, or “moodiness.”
They are biological rhythms interacting with real life.
Supporting a partner through their cycle doesn’t require fixing anything. What often helps most is curiosity, patience, and emotional presence.
During the Menstrual Phase (Rest & Reflection)
Your partner may have less energy, increased pain, or heightened emotional sensitivity during this time.
What can help:
- Normalize rest without guilt (“It makes sense you’re tired.”)
- Offer practical support (meals, chores, quiet companionship)
- Ask before offering solutions
- Respect a need for space or reduced stimulation
Helpful mindset:
This is a time for gentleness, not productivity.
During the Follicular Phase (Energy & Momentum)
As energy returns, your partner may feel more motivated, social, and mentally clear.
What can help:
- Encourage goals and new ideas
- Join in activities they enjoy
- Share excitement without pressuring them to do everything
- Appreciate their creativity and enthusiasm
Helpful mindset:
This is a time to build together.
During Ovulation (Connection & Confidence)
Many people feel more confident, expressive, and relational during this phase.
What can help:
- Engage in meaningful conversations
- Plan social or intimate time if desired
- Affirm strengths and contributions
- Stay attuned to signs of overstimulation or anxiety
Helpful mindset:
This is a time for connection and affirmation.
During the Luteal Phase (Sensitivity & Support)
This phase often comes with increased emotional intensity, fatigue, or stress sensitivity.
What can help:
- Practice patience during mood shifts
- Avoid minimizing feelings (“You’re overreacting” can be deeply harmful)
- Offer reassurance and emotional safety
- Reduce conflict when possible and revisit difficult topics later
- Encourage rest and grounding activities
Helpful mindset:
This is a time for compassion, not correction.
What Partners Often Get Wrong (and How to Reframe)
- ❌ “You’re being dramatic.”
✔️ “I can see this feels really hard right now.” - ❌ “It’s just hormones.”
✔️ “Your feelings matter, regardless of the cause.” - ❌ Trying to fix everything
✔️ Asking, “Do you want comfort, space, or help?”
Support does not mean walking on eggshells—it means responding with empathy rather than judgment.
Questions Partners Can Gently Ask
- “What feels most supportive for you right now?”
- “Do you want company or quiet?”
- “Is there anything I can take off your plate today?”
- “Would it help to talk, or would rest feel better?”
These questions communicate care while respecting autonomy.
Keep in Mind
Menstrual cycles are not excuses—they are contexts. Understanding that context allows relationships to move from frustration to collaboration.
When partners learn the rhythm together, it often reduces conflict, increases emotional safety, and builds trust. You’re not managing symptoms—you’re supporting a whole person.
Hormones influence capacity, not character.
Emotions are signals, not problems.
Repair matters more than perfection.
Learning to communicate through the menstrual cycle isn’t about avoiding conflict—it’s about navigating it with care, timing, and respect.
Below are some Scripts conducting difficult conversations:
Supportive language for partners navigating hormonal shifts, emotions, and misunderstandings
Difficult moments don’t mean a relationship is failing—they usually mean two nervous systems are under stress at the same time. Having language ready can reduce defensiveness and help both people feel safer.
These scripts aren’t meant to be followed perfectly. They’re examples of tone, pacing, and intention. Adjust them so they sound like you.
When Your Partner Is More Emotionally Sensitive Than Usual
Instead of:
“You’re being really emotional right now.”
Try:
“I can tell things feel heavier today. I want to understand what you’re experiencing—do you want to talk, or would comfort help more?”
Why this helps:
It names the emotional shift without judgment and gives your partner choice.
When You’re Not Sure If It’s a ‘Cycle Thing’ or a Real Issue
Instead of:
“Is this just PMS?”
Try:
“I want to take what you’re feeling seriously. Even if timing is part of it, I care about what’s coming up for you.”
Why this helps:
It separates validation from cause and avoids dismissing the concern.
When Conflict Is Escalating During the Luteal or Menstrual Phase
Try:
“I care about this conversation, and I also notice we’re both feeling overwhelmed. Could we pause and come back to this when we’re more resourced?”
Why this helps:
It prioritizes emotional safety without avoiding the issue.
When You Need to Set a Boundary Without Sounding Dismissive
Try:
“I want to support you, and I’m also feeling stretched right now. Can we checkin about what kind of support would feel most helpful—for both of us?”
Why this helps:
It balances empathy with honesty and reduces resentment.
When Your Partner Wants Space
Try:
“I hear that you need space. I’m here when you’re ready, and I won’t take the distance personally.”
Why this helps:
It reassures connection while respecting autonomy.
When You’ve Said Something Hurtful and Want to Repair
Try:
“I’ve been thinking about what I said earlier. I see how it could have felt invalidating, and I’m sorry. That wasn’t my intention.”
Why this helps:
It focuses on impact rather than defensiveness.
When You Feel Confused or Shut Out
Try:
“I’m feeling a bit disconnected and unsure how to help. Could you tell me what feels most supportive right now—or what doesn’t?”
Why this helps:
It invites collaboration rather than guessing.
When a Partner Wants Solutions but the Other Needs Validation
Try:
“Before I offer ideas, do you want empathy, problem-solving, or just someone to sit with you?”
Why this helps:
It prevents well-meaning advice from feeling invalidating.
When You Want to Name the Cycle Without Blame
Try:
“I notice this phase of the month can be more intense for you. How can I show up in a way that feels supportive right now?”
Why this helps:
It acknowledges patterns without reducing the person to hormones.
For the Menstruating Partner: Advocating for Your Needs
These scripts can help you express needs clearly without apologizing for them.
- “This phase is harder on my energy. I need more rest and less pressure right now.”
- “I’m more emotionally sensitive today—reassurance helps more than solutions.”
- “I care about this issue, and I’ll be able to talk about it more clearly in a few days.”
- “What I need right now is comfort, not fixing.”
Your needs are not inconvenient—they are information.
References
Tava Health. (2025, February 13). UnderstandingWomen’s Mental Health: How hormones
impact mood and well-being.Tava Health. <ahref="https:>https://www.tavahealth.com/resources/womens-mental-health-hormones</ahref="https:>
Cleveland Clinic. (2022, December 9). Menstrualcycle. Cleveland Clinic.
<ahref="https:>https://my.clevelandclinic.org/health/articles/10132-menstrual-cycle</ahref="https:><ahref="https:>m</ahref="https:>
Forte, N.,Harris, MD, MA, FAPA, P., & Basheda, V. (n.d.). How your menstrual cycle affects your behavior. EverydayHealth.com.https://www.everydayhealth.com/womens-health/how- your-menstrual-cycle-affects-your-behavior.aspx#how-diet-impacts-menstrual-cramps
